HSV 1/2 IGG HERPES SELECT with Reflex
What is genital herpes?
Genital Herpes is an STD caused by two types of viruses. The viruses are called herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2).
Symptoms of genital herpes?
Most people who have genital herpes have no symptoms, or have very mild symptoms. You may not notice mild symptoms or you may mistake them for another skin condition, such as a pimple or ingrown hair. Because of this, most people who have herpes do not know it.
Herpes sores usually appear as one or more blisters on or around the genitals, rectum or mouth. The blisters break and leave painful sores that may take a week or more to heal. These symptoms are sometimes called “having an outbreak.” The first time someone has an outbreak they may also have flu-like symptoms such as fever, body aches, or swollen glands.
People who experience an initial outbreak of herpes can have repeated outbreaks, especially if they are infected with HSV-2. Repeat outbreaks are usually shorter and less severe than the first outbreak. Although the infection stays in the body for the rest of your life, the number of outbreaks may decrease over time.
- an unusual sore
- a smelly genital discharge
- burning when urinating, or (for women) bleeding between periods.
- blisters around genitals, rectum or mouth
- First outbreak flu-like symptoms such as fever, body aches or swollen glands
What is oral herpes?
Oral herpes is usually caused by HSV-1 and can result in cold sores or fever blisters on or around the mouth. However, most people do not have any symptoms. Most people with oral herpes were infected during childhood or young adulthood from non-sexual contact with saliva.
Is there a link between genital herpes and oral herpes?
Oral herpes caused by HSV-1 can be spread from the mouth to the genitals through oral sex. This is why some cases of genital herpes are caused by HSV-1.
How common is genital herpes?
Genital herpes is common in the United States. More than one out of every six people aged 14 to 49 years have genital herpes.
How is genital herpes spread?
You can get genital herpes by having vaginal, anal, or oral sex with someone who has the disease.
If you do not have herpes, you can get infected if you come into contact with the herpes virus in:
- A herpes sore;
- Saliva (if your partner has an oral herpes infection) or genital secretions (if your partner has a genital herpes infection);
- Skin in the oral area if your partner has an oral herpes infection, or skin in the genital area if your partner has a genital herpes infection.
You can get herpes from a sex partner who does not have a visible sore or who may not know he or she is infected. It is also possible to get genital herpes if you receive oral sex from a sex partner who has oral herpes.
You will not get herpes from toilet seats, bedding, or swimming pools, or from touching objects around you such as silverware, soap, or towels. If you have additional questions about how herpes is spread, consider discussing your concerns with a healthcare provider.
How can I reduce my risk of getting genital herpes?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting genital herpes:
- Be in a long-term mutually monogamous relationship with a partner who is not infected with an STD (e.g., a partner who has been tested and has negative STD test results);
- Using latex condoms the right way every time you have sex.
Be aware that not all herpes sores occur in areas that are covered by a latex condom. Also, herpes virus can be released (shed) from areas of the skin that do not have a visible herpes sore. For these reasons, condoms may not fully protect you from getting herpes.
If you are in a relationship with a person known to have genital herpes, you can lower your risk of getting genital herpes if:
- Your partner takes an anti-herpes medication every day. This is something your partner should discuss with his or her doctor.
- You avoid having vaginal, anal, or oral sex when your partner has herpes symptoms (i.e., when your partner is having an outbreak).
I’m pregnant. How could genital herpes affect my baby?
If you are pregnant and have genital herpes, it is very important for you to go to prenatal care visits. Tell your doctor if you have ever had symptoms of, or have been diagnosed with, genital herpes. Also tell your doctor if you have ever been exposed to genital herpes. There is some research that suggests that genital herpes infection may lead to miscarriage, or could make it more likely for you to deliver your baby too early.
Herpes infection can be passed from you to your unborn child before birth but is more commonly passed to your infant during delivery. This can lead to a potentially deadly infection in your baby (called neonatal herpes). It is important that you avoid getting herpes during pregnancy. If you are pregnant and have genital herpes, you may be offered anti-herpes medicine towards the end of your pregnancy. This medicine may reduce your risk of having signs or symptoms of genital herpes at the time of delivery. At the time of delivery, your doctor should carefully examine you for herpes sores. If you have herpes symptoms at delivery, a ‘C-section’ is usually performed.
How will my doctor know if I have herpes?
Your healthcare provider may diagnose genital herpes by simply looking at your symptoms. Providers can also take a sample from the sore(s) and test it. In certain situations, a blood test may be used to look for herpes antibodies. Have an honest and open talk with your health care provider and ask whether you should be tested for herpes or other STDs.
Please note: A herpes blood test can help determine if you have herpes infection. It cannot tell you who gave you the infection or how long you have been infected.
Can herpes be cured?
There is no cure for herpes. However, there are medicines that can prevent or shorten outbreaks. One of these anti-herpes medicines can be taken daily, and makes it less likely that you will pass the infection on to your sex partner(s).
What happens if I don’t get treated?
Genital herpes can cause painful genital sores and can be severe in people with suppressed immune systems.
If you touch your sores or the fluids from the sores, you may transfer herpes to another part of your body, such as your eyes. Do not touch the sores or fluids to avoid spreading herpes to another part of your body. If you do touch the sores or fluids, immediately wash your hands thoroughly to help avoid spreading your infection.
If you are pregnant, there can be problems for you and your developing fetus, or newborn baby. See “I’m pregnant. How could genital herpes affect my baby?” above for information about this.
Can I still have sex if I have herpes?
If you have herpes, you should talk to your sex partner(s) and let him or her know that you do and the risk involved. Using condoms may help lower this risk but it will not get rid of the risk completely. Having sores or other symptoms of herpes can increase your risk of spreading the disease. Even if you do not have any symptoms, you can still infect your sex partners.
You may have concerns about how genital herpes will impact your overall health, sex life, and relationships. It is best for you to talk to a health care provider about those concerns, but it also is important to recognize that while herpes is not curable, it can be managed with medication. Daily suppressive therapy (i.e., daily use of antiviral medication) for herpes can also lower your risk of spreading genital herpes to your sex partner. Be sure to discuss treatment options with your healthcare provider. Since a genital herpes diagnosis may affect how you will feel about current or future sexual relationships, it is important to understand how to talk to sexual partners about STDs.
What is the link between genital herpes and HIV?
Herpes infection can cause sores or breaks in the skin or lining of the mouth, vagina, and rectum. This provides a way for HIV to enter the body. Even without visible sores, having genital herpes increases the number of CD4 cells (the cells that HIV targets for entry into the body) found in the lining of the genitals. When a person has both HIV and genital herpes, the chances are higher that HIV will be spread to an HIV-uninfected sex partner during sexual contact with their partner’s mouth, vagina, or rectum.
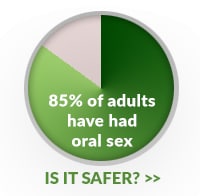
Is Oral Sex Safer than Vaginal or Anal Sex?

- Many STDs can be spread through oral sex. However, it is difficult to compare the exact risks of getting specific STDs from specific types of sexual activity. This is partly because most people who have oral sex also have vaginal or anal sex. Also, few studies have looked at the risks of getting STDs other than HIV from giving oral sex on the vagina or anus, compared to giving oral sex on the penis.
- Studies have shown that the risk of getting HIV from having oral sex with an infected partner (either giving or getting oral sex) is much lower than the risk of getting HIV from anal or vaginal sex with an infected partner. This may not be true for other STDs – in one study of gay men with syphilis, 1 out of 5 reported having only oral sex.
- Getting HIV from oral sex may be less likely than vaginal or anal sex, but it still carries risk. If you are having oral sex you should still protect yourself. Repeated unprotected oral sex exposure to HIV may represent a considerable risk for spread of HIV, as well as other STDs for which the risk of spread through oral sex has not been as well studied.
- It is possible that getting certain STDs, such as chlamydia or gonorrhea, in the throat may not pose as great a threat to an infected person’s health as getting an STD in the genital area or rectum. Having these infections in the throat might increase the risk of getting HIV. Having gonorrhea in the throat also may lead to spread of the disease throughout the body. In addition:
- Having infections of chlamydia and gonorrhea in the throat may make it easier to spread these infections to others through oral sex. This is especially important for gonorrhea, since throat infections are harder to treat than urinary, genital or rectal infections.
- Infections from certain STDs, such as syphilis and HIV, spread throughout the body. Therefore, infections that are acquired in the throat may lead to the same health problems as infections acquired in the genitals or rectum.
- Mouth and throat infections by certain types of HPV may develop into oral or neck cancer.
What May Increase the Chances of Giving or Getting an STD through Oral Sex?
It is possible that certain factors may increase a person’s chances of getting HIV or other STDs during oral sex if exposed to an infected partner, such as:
- Having poor oral health which can include tooth decay, gum disease or bleeding gums, and oral cancer.
- Having sores in the mouth or on the genitals.
- Being exposed to the “pre-cum” or “cum” (also known as pre-ejaculate or ejaculate) of an infected partner.
However, no scientific studies have been done to show whether or not these factors actually do increase the risk of getting HIV or STDs from oral sex.
What Can You Do to Prevent STD Transmission During Oral Sex?
You can lower your chances of giving or getting STDs during oral sex by using a condom, dental dam or other barrier method each and every time you have oral sex.
- For oral sex on the penis:
- Cover the penis with a non-lubricated latex condom.
- Use plastic (polyurethane) condoms if you or your partner is allergic to latex.
- For oral sex on the vagina or anus:
- Use a dental dam.
- Cut open a condom to make a square, and put it between the mouth and the partner’s vagina or anus.
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting an STD:
- Being in a long-term mutually monogamous relationship with a partner who is not infected with an STD (e.g., a partner who has been tested and has negative STD test results).
- Using latex condoms the right way every time you have sex.
It’s important to remember that many infected individuals may be unaware of their infection because STDs often have no symptoms and are unrecognized.
If you are sexually active, you should get tested regularly for STDs and HIV and talk to your partner(s) about STDs. If you think you might have an STD, stop having sex and get tested today. It is important that you talk openly with your healthcare provider about any activities that might put you at risk for an STD, including oral sex.

